Hyperthyroidism in cats and dogs
What is hyperthyroidism in cats and dogs?
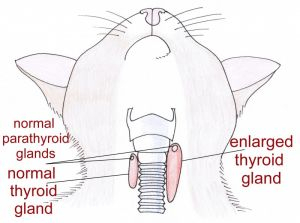
The thyroid is a two-lobed gland located in the neck. It produces hormones, known as T3 and T4, which regulate the body’s metabolism and affect many processes of the body. If too little thyroid hormone is produced, the processes become sluggish; if too much is produced, the processes run too fast.
Hyperthyroidism is characterised by an enlarged thyroid gland that produces an excess of thyroid hormones (in medical terms, “hyper-“ means high, beyond, excessive or above normal). Overactivity of the thyroid gland is a common feline disease – it is in fact the most common hormone imbalance occurring in cats. It rarely occurs in dogs; when a dog is afflicted, it is usually serious.
Source: https://www.vethospital.co.nz/post/hyperthyrodism-in-cats
Hyperthyroidism can occur in any breed of cat, male or female, and almost exclusively affects middle-aged and older felines. Less than 6 percent of cases are younger than 10 years of age; the average age at onset is between 12 and 13 years. About 70% of cats have both lobes of the thyroid gland affected.
Because the thyroid hormones affect nearly all the organs in the body, thyroid disease often causes secondary problems. Raised thyroid hormones stimulate an increased heart rate and a stronger contraction of the heart muscle and can eventually cause thickening of the heart’s left ventricle. If left unmanaged, these changes may eventually compromise the normal function of the heart, leading to secondary heart disease or heart failure. Hypertension, or high blood pressure, is another potential complication of hyperthyroidism, which can cause additional damage to the organs, including the eyes, kidneys, heart, and brain.
Symptoms of hyperthyroidism in cats and dogs
Thyroid hormones are responsible for regulating many body processes. When too much of it is produced, the clinical signs can be quite notable, and the animal can become seriously ill. The hallmark sign is weight loss despite excellent appetite. Thyroid hormones help control the body’s metabolic rate and cats and dogs with hyperthyroidism tend to burn up energy too rapidly, typically suffering weight loss despite having an increased appetite and increased food intake.
Physical symptoms in cats
Cats afflicted with hyperthyroidism usually develop a variety of signs that may be subtle at first but that become more severe as the disease progresses, including:
- Weight loss (seen in 95 to 98 % of cases)
- Insatiable appetite (seen in 67 to 81% of cases)
- Excessive thirst
- Increased urination
- Unkempt, matted or greasy coat
- Hair loss
- Panting
- Diarrhoea
- Increased shedding
- Vomiting (occurs in about 50 percent of affected cats)
- Increased heart rate

Hyperthyroid cats are often extra thirsty and may be brought to the vet because they are drinking so much water. They are commonly restless and especially demanding of attention and/or food. Many have chronic intermittent vomiting or diarrhoea and may be urinating in inappropriate locations.
Behavioural symptoms in cats
The association between thyroid dysfunction and behavioural changes has long been recognised. Cats with hyperthyroidism may engage in bizarre and abnormal behaviours; for example, affected cats are often hyperactive and restless and may become cranky or aggressive. After an episode, many cats appear to come out of a trance-like state and are unaware of their peculiar behaviour.
Behavioural symptoms in cats may include:
- Unprovoked aggression towards other animals and/or people
- Sudden onset of seizure disorder in adulthood
- Disorientation
- Moodiness
- Erratic temperament
- Periods of hyperactivity
- Increased vocalizing, particularly at night
- Hypo attentiveness
- Depression
- Fearfulness and phobias
- Anxiety
- Submissiveness
- Passivity
- Compulsiveness
- Irritability
- Listlessness
- Nervousness

Symptoms in dogs
Dogs with hyperthyroidism exhibit similar symptoms that reflect an increased metabolic rate, including weight loss, increased appetite and thirst, increased urination, hyperactivity and increased heart rate. As well as these symptoms, the dog’s owner often discovers a lump on the dog’s neck in the vicinity of the thyroid glands.
Causes of hyperthyroidism in cats and dogs
Causes in cats
Hyperthyroidism is caused by an increase in production of thyroid hormones (known as T3 and T4) from an enlarged thyroid gland in the neck. In cats, the most common cause of enlarged thyroid glands, occurring in almost 98% of cases, is a non-cancerous tumour called an adenoma that interferes with the functioning of the gland. Some rare cases (less than 3%) are caused by malignant tumours known as thyroid adenocarcinomas.
Contributing factors to feline hyperthyroidism are thought to include lifestyle factors, deficiencies or excesses of certain compounds in the diet and chronic exposure to thyroid-disrupting chemicals in food or the environment. An indoor lifestyle has been correlated with increased chance of a cat being diagnosed with hyperthyroidism. This has led to a range of theories as to why this is, including:
- A chemical found in cat litter
- A household chemical
- The greater likelihood of indoor cats reaching the age at which hyperthyroidism develops.
- Indoor cats are more likely to see the vet and have diagnostic testing while outdoor cats simply go undiagnosed.
Purebred cats, especially the Siamese and Himalayan breeds, appear to have a decreased incidence of hyperthyroidism (i.e., they are less likely to develop this condition). This implies that there may be genetic factors at work as well.
Causes in dogs
In dogs, although occurring rarely, the most likely cause is a malignant carcinoma. This is a cancerous tumour occurring in the thyroid gland which interferes with the normal functioning of the thyroid, prompting it to produce excessive hormones. The condition may also result from medication prescribed to counter hypothyroidism, a condition characterised by the underproduction of thyroid hormones.
How is hyperthyroidism in cats and dogs diagnosed?
Diagnosis in cats
A veterinarian who suspects a cat has a thyroid problem will conduct a physical examination and palpate the cat’s neck area to check for an enlarged thyroid gland. In a normal cat, the lobes of the thyroid gland cannot be felt with the fingers, but in the hyperthyroid cat, at least one lobe is usually prominent and may be detected by the vet.

Since hyperthyroidism can predispose a cat to other conditions, it is important to evaluate general health, particularly the heart and kidneys. The vet will probably order a complete blood count (CBC), chemistry panel and urinalysis and an analysis of thyroid hormone levels.
A blood chemistry panel, CBC and urinalysis will provide information about the heart, kidneys and other organs and provide your veterinarian with an overall picture of your cat’s health, and while they will not provide a definitive diagnosis of hyperthyroidism, they can rule out diabetes and kidney failure. Hyperthyroid cats may have normal findings on the CBC and urinalysis, but the chemistry panel often shows increases in several liver enzymes that indicate mild damage to the liver and/or bones.
In most cases, a definitive diagnosis of hyperthyroidism is based on a simple blood test that shows elevated T4 levels in the bloodstream. If T4 is markedly elevated, the diagnosis is clear and there can be no other diagnosis in this event. However, between 2 percent and 10 percent of cats with hyperthyroidism will have normal or borderline T4 levels and require further testing if the vet still suspects hyperthyroidism.
Diagnosis in dogs
In dogs, a preliminary diagnosis of hyperthyroidism can often be made after palpitation of the thyroid gland, where a thyroid mass is detected. While a battery of tests may be required for a definitive diagnosis, standard tests will include a chemical blood profile, a complete blood count and a urinalysis. A diagnosis can be confirmed by a high concentration of T4 in the blood serum, which is the most common finding of the profile. In some cases, however, the T4 levels may be in the normal range, making a diagnosis more difficult, particularly in the early stages of this disease. If the blood tests are not conclusive, further tests will be required. Thyroid issues can sometimes be secondary to other illnesses so these tests will help rule out or confirm this possibility.
Diagnostic imaging can be utilised to fully understand the extent of the thyroid mass. An ultrasound can show if there is a thickened area around the thyroid glands or in the area distal to the larynx (voice box). It can verify the location and the depth of the mass as well as help the vet with the treatment plan. Imaging of the chest and heart may be useful in assessing if the dog is experiencing any heart abnormalities and to check for pulmonary metastasis (spread of the cancer into the lungs).
Prognosis
Cat prognosis
The prognosis for cats with hyperthyroidism is generally good, if they are receiving appropriate therapy. Hyperthyroid cats may experience reduced quality of life because of weight loss, muscle deterioration, chronic vomiting and/or chronic diarrhoea. Because of the important role the thyroid gland plays in the body, some cats with hyperthyroidism develop secondary problems, including heart disease and high blood pressure. If complications involving other organs exist, the prognosis may worsen. Fortunately, most cats that develop hyperthyroidism can be treated very successfully and will make a complete recovery.
Dog prognosis
Because canine hyperthyroidism is almost always associated with thyroid carcinoma, the long-term prognosis in affected dogs is poor to grave. Malignant tumours of this type often metastasize quickly into the surrounding tissues and organs, making treatment difficult or impossible. If detected early, when the mass is small, there is a much better chance of recovery. Benign tumours can generally be managed and have a much better prognosis.
Treatment of hyperthyroidism in cats and dogs
Treatment for cats
There are four treatment options for feline hyperthyroidism, each with advantages and disadvantages. The treatment recommended by your vet will depend on your cat’s specific circumstances, including his or her overall health status, your own ability and willingness to medicate the cat regularly, and financial considerations.
Even if your cat is not experiencing obvious symptoms at the time of diagnosis, there are less visible reasons to proceed with treatment, including heart disease and high blood pressure. These conditions, which can result in heart failure, sudden blindness, or even sudden death, can be prevented with timely and appropriate treatment for hyperthyroidism.
Medication
The drug of choice for hyperthyroidism in cats is Methimazole, an anti-thyroid drug that reduces the production and release of thyroid hormone from the thyroid gland. It is highly effective in correcting the condition, often within two to three weeks. While medication does not cure the hyperthyroidism, it does allow for short-term or long-term control of the disease.
The advantages of medication are that the drugs are readily available and relatively inexpensive. However, some cats experience adverse reactions to the medication, including vomiting, loss of appetite, anaemia, depression and bleeding. Daily or twice-daily oral dosage will usually be required, and for some owners and cats, this schedule may be difficult to maintain. Blood tests will be conducted periodically during treatment to evaluate whether the therapy is effective and to monitor kidney function and for potential side effects.

Radioactive iodine therapy
This is a safe and very effective treatment for feline hyperthyroidism, and the therefore the treatment of choice where it is available. Radioactive iodine may be administered to the cat by injection or capsule. As iodine is required to produce T3 and T4, the radioiodine becomes concentrated in the thyroid tumour, where it emits radiation and destroys the hyperfunctioning thyroid tissue without damaging other structures. No anaesthesia or surgery is required, and cure rates approximately 95 to 98% with one treatment.
On the negative side, it involves a stay in hospital in a special lead-lined room until the level of radioactivity in the cat has fallen to an acceptable level that is deemed safe – usually 7 to 10 days. Also, radioiodine therapy is costly and may therefore be out of reach for many cat owners.
Surgery
Surgical removal of the thyroid gland (unilateral) or glands (bilateral), known as thyroidectomy, is an effective and straightforward procedure. Surgery usually results in a cure, but anaesthesia can be challenging and cause complications in older cats and those whose disease may have affected their hearts, kidneys and other organs. Another major risk is inadvertent injury to the nearby parathyroid glands, which regulate the calcium levels in the blood. Because medication and radioactive iodine therapy are just as successful yet less invasive therapies, surgery is not as commonly the treatment of choice for the condition.
Dietary therapy
Limiting dietary iodine intake is a fourth treatment option for feline hyperthyroidism. Thyroid hormones T3 and T4 are made with iodine, therefore, the production of excessive amounts of thyroid hormone cannot occur without iodine. Since iodine comes from the diet, an iodine-restricted diet will preclude production of excessive amounts of T3 and T4 without resulting in an iodine deficiency.
While limited-iodine diets have been available commercially since 2011 (e.g. Hill’s Prescription Diet Y/D), research into this form of treatment is still ongoing, with concerns over the effects of long-term iodine restriction on health and the possibility that it may cause the hyperthyroidism to worsen. Cats must eat this diet exclusively with no supplementation with other foods, treats, or hunting. Whether this diet is appropriate and manageable for your cat, and whether it should replace other therapies, should always be discussed with your vet before proceeding.
Treatment for dogs
In dogs diagnosed with thyroid carcinoma as the primary cause of hyperthyroidism, the treatment options will depend on the stage of the cancer, the size of the tumour and whether the cancer has spread (metastasized) into nearby tissue or other areas of the body. Treatment options include surgery, radiation therapy, chemotherapy and radioactive iodine are potential treatment options. In these cases, medications may improve the symptoms of hyperthyroidism but will not treat the underlying tumour.
Overview
Hyperthyroidism is a common disease of older cats with the average age at diagnosis being around 13-years. It is a rare but serious condition in dogs, usually resulting from a malignant thyroid tumour. The condition is characterised by an increase in production of thyroid hormones from the thyroid glands, which are situated in the neck. Weight loss and increased appetite are among the most common symptoms of this condition.
Fortunately, most cats that develop hyperthyroidism can be treated very successfully and make a complete recovery. Four treatment options are available – antithyroid medications that interfere with the production of thyroid hormones (methimazole), surgical thyroidectomy, administration of radioactive iodine, or nutritional management with a low-iodine diet. Prognosis is generally good, with most affected cats responding well to treatment, although cats with severe disease involving many systems may not survive. For dogs with a thyroid carcinoma as the primary cause, the prognosis is less optimistic. If the tumour is detected early, there is a greater chance of successful treatment and outcome.
Bow Wow Meow Pet Insurance can help protect you and your pet should an unexpected trip to the vet occur.
-
Find out more about our dog insurance options
-
Find out more about our cat insurance options
-
Get an instant online pet insurance quote


Learn more:
- https://pets.webmd.com/cats/guide/cat-hyperthyroidism#1
- https://www.vet.cornell.edu/departments-centers-and-institutes/cornell-feline-health-center/health-information/feline-health-topics/hyperthyroidism-cats
- https://www.vet.cornell.edu/hospitals/companion-animal-hospital/internal-medicine/feline-hyperthyroidism
- https://pets.webmd.com/cats/guide/cat-hyperthyroidism
- https://veterinarypartner.vin.com/default.aspx?pid=19239&id=4951397
- https://veterinarypartner.vin.com/default.aspx?pid=19239&id=4951398\
- https://veterinarypartner.vin.com/default.aspx?pid=19239&id=5305366
- https://www.msdvetmanual.com/endocrine-system/the-thyroid-gland/hyperthyroidism-in-animals
- https://www.msdvetmanual.com/cat-owners/hormonal-disorders-of-cats/disorders-of-the-thyroid-gland-in-cats
- https://www.msdvetmanual.com/dog-owners/hormonal-disorders-of-dogs/disorders-of-the-thyroid-gland-in-dogs
- https://www.akc.org/expert-advice/health/thyroid-disease-in-dogs/
- https://www.petmd.com/dog/conditions/endocrine/c_dg_hyperthyroidism
- https://wagwalking.com/condition/hyperthyroidism
- https://ivcjournal.com/thyroid-dysfunction-aberrant-behavior/






